Osteoarthritis(Arthropathy) is a joint disease characterized by degenerative changes in the cartilage covering the bones, in other words, destruction.
%20and%20normal%20cartilage%20(right).jpg)
The vast majority of affected joints are knee joints, hip joints, shoulder joints and first metatarsophalangeal joints. Damage to other joints is less common and is usually secondary. In recent years, the disability caused by osteoarthritis has doubled.
Like any disease, osteoarthritis has risk factors for its development. These factors are being actively studied today, and the list is expanding every year. Mainly considered to be:
- age;
- Genetic
- Metabolic disorders;
- Weight gain
- Osteoporosis;
- Undernourishment and irregularities;
- Endocrine disorders;
- menopause;
- Often hypothermia;
- trauma;
- Arthritis (inflammation of the joints);
- A focus of chronic infection or inflammation (for example, chronic tonsillitis).
- Varicose veins.
If you notice similar symptoms, please consult your doctor. Do not self-medicate-it is harmful to your health!
Osteoarthritis symptoms
Common symptoms of joint disease include:
- Pain when tired;
- Limited joint movement;
- Feeling stiff in the morning, "crunchy" feeling;
- Pain after prolonged rest (the so-called "start").
Joint pain is rarely acute, more commonly painful or dull, and usually stops at rest. Symptoms are usually wavy and can come and go without trying to treat them. They can be mild, moderate or severe. Over the years, complaints of osteoarthritis may remain roughly the same, but over time they will progress and the condition will worsen. Mild and moderate symptoms can be controlled at the same level, but the serious course of the disease can lead to chronic pain and inability to carry out daily housework activities, which can lead to disability up to disability.
Pathogenesis of osteoarthritis
The main nutrient medium for joints is synovial fluid. It also acts as a lubricant between the joint surfaces. The metabolic processes in the joints and their structures play an important role in the development of osteoarthritis. In the initial stage, when a biochemical disorder appears in synovial fluid, its nature will decrease, triggering the destruction mechanism. The first thing that is impacted is the synovial membrane of the joint. It plays an important role as a membrane. It is a filter of hyaluronic acid, the most important nutrient of the cartilage, to prevent it from leaving its main workplace-the joint. Cavity. The saturation of the characteristics of joint fluid determines its circulation, which is inseparable from the regular movement of the joint itself. Therefore, the famous phrase "movement is life". The continuous circulation of synovial fluid in the joint cavity is the key to its full metabolism. Due to lack of nutrients, cartilage becomes thinner, the formation of new cells stops, and the joint surface becomes uneven, rough, and defective areas. The relationship between venous diseases of the lower extremities (such as varicose veins) and the development of metabolic disorders in the joints (mainly the knee joint) is known. The subchondral bone structure responds to this process with a compensatory mechanism-thickening, thickening, and expanding the coverage area, leading to the formation of exogenous osteophytes and osteophytes, which are the main reasons for joint limitation and deformity. The synovial fluid is full of inflammatory cells and decaying elements. The joint capsules that respond to this thicken, become rough and lose their elasticity, and the soft tissues become dry (dehydration occurs). Therefore, morning stiffness and "start pain" occur. The pathological process in the final stage prompts the body to turn on the final compensatory mechanism—brake. At rest and in the so-called physiological position, soreness is minimal, and the ligament apparatus is maximized. In this position, the joint tends to fix itself, and it succeeds in quickly forming a thicker exogenous bone, thereby "fixing" the joint, and the patient loses the ability to move it completely. The muscles of this limb atrophy and become weaker and weaker. This change has been considered irreversible.
Classification and stages of development of osteoarthritis
The disease is divided into two categories: primary (or idiopathic) and secondary. The first group developed due to unknown reasons or age-related changes. The second is characterized by a clear cause and as a result of its pathological process (for example, in the context of tuberculosis, osteochondrosis dissecans, subchondral necrosis, etc. )
No matter what causes the development of osteoarthritis, its development has 4 stages:
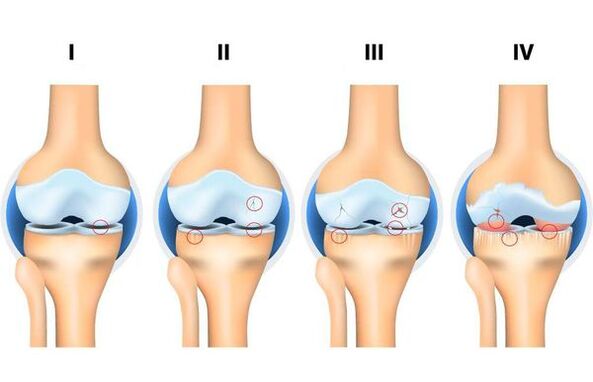
- The first stage: The hard structure of the joint does not participate in the destruction process, and the composition of its soft structure and joint fluid (which is a nutrient medium that reduces joint friction) has a preliminary change, and there is a joint dystrophy.
- Phase 2: Accompanied by the "start" of the destruction mechanism of the joint solid structure, the marginal solid structure (exogenous osteophytes, osteophytes) is formed. Moderate complaints about changes in range of motion.
- Stage 3: Accompanying the narrowing of the joint cavity, the load surface is obviously damaged, osteochondral defects are formed, movement is obviously restricted, there is a constant "crunchy" feeling during the movement, and the initial change of the limb axis.
- Stage 4: Severe, in which the movement of the joint is obviously restricted until it is completely absent (stiffness), obvious inflammatory process, its deformation, the formation of bone defects (due to the complete lack of cartilage coverage).
Complications of osteoarthritis
Without treatment, any disease can cause complications, and joint disease is no exception. If this is the main form, then the main complications include:
- Damage to the soft structure of the joint (degenerative meniscus tear, ligament rupture, etc. );
- Chronic inflammatory process;
- Ankylosis (no movement of the joint at all);
- The joint is deformed.
If this is a secondary form, the complications depend on the process leading to the development of arthropathy. For example, it may cause osteoporosis, a chronic disease characterized by progressive disorders of bone metabolism. As a result, bones become fragile and nutrition is disturbed, thereby complicating osteoarthritis due to the threat of intra-articular fractures. Therefore, it is very important to seek medical treatment in time. As the famous surgeon wrote: "The future belongs to preventive medicine. "
Diagnosis of osteoarthritis
The diagnosis of joint disease usually starts with a doctor (usually an orthopedic traumatologist) in the first-line medical (polyclinic), where clinical examinations are performed and the examination data (CT, MRI, X-rays, etc. ) are interpreted to determine the degree of osteoarthritisAnd type. . . Diagnosis and diagnosis are usually simple. If the diagnosis is not clear or the doctor recommends the secondary development of the disease, then for clarification, the patient will be referred to another professional doctor (for example, a rheumatologist). If there is no test result, it is difficult to determine the degree of joint disease. Disease history, methods, and treatment attempts are also important for diagnosis and determination of treatment strategies, because doctors often face the difficult task of differential diagnosis (for example, symptoms of joint disease and arthritis often overlap).
Osteoarthritis treatment
It provides a comprehensive approach in the initial stage of osteoarthritis suitable for conservative treatment. Treatment takes a long time and the main goal is pursued: either stop the destruction process at the beginning of the treatment, or slow it down. The complex includes drug and non-drug treatments, including exercise therapy (physical therapy and gymnastics), physical therapy (usually sonic therapy and magnetic therapy), swimming, anti-inflammatory therapy (ingested or topical in the form of gel or cream)) Courses, chondroprotective therapy (taking cartilage-based medicines) and intra-articular injections (these can be homeopathic medicines and hyaluronic acid preparations). Orthopedic traumatologists are still using chondroprotective agents, which are prescribed by internal curricula, but recent scientific research results in Western countries refute the positive effects compared to the placebo effect. The symptoms are serious, the stage is serious, conservative treatment is ineffective, and surgical treatment is the first priority. Given the indications, it can be minimally invasive treatment-arthroscopy and endoprosthesis. Arthroscopy (arthroscope) is sterilized under the control of a video optical system to remove exogenous bone (if possible) and soft structure damage, which is usually observed at these stages. However, recently, the benefits of this type of osteoarthritis intervention have been increasingly questioned because it does not have the expected effect in chronic pain and in some cases, if not performed properly, it may cause major harm.
Endoprosthesis is a technically difficult and difficult operation. Its purpose is to create an artificial and brand new joint. In the presence of contraindications, clear indications and risk identification are required. Today, endoprostheses for knee joints, hip joints and shoulder joints have been successfully used. The doctor's further outpatient supervision reduces the risks and conditions of rehabilitation, and improves the quality and efficiency of the operation.
forecast. prevention
The prediction depends on timely visits to traumatologists and orthopedic surgeons and the start of comprehensive treatment. In terms of eliminating the morphological changes of osteoarthritis, the prognosis is unfavorable because it is impossible to completely restore the cartilage structure of the joint. In old age, the course of the disease is more serious than in young people. However, by seeing a doctor in time and following all recommendations, all complaints can be eliminated and the full motion function of the joint can be restored.
Precaution:
- Exercise regularly.It is a misunderstanding that physical activity can "wear out" joints. Increase-yes, but not regularly and moderately. According to the latest data, any activity designed to strengthen and maintain muscle mass, improve coordination, and support joint motor function and blood supply. Any physical activity can allow you to achieve the normal circulation of joint fluid, which is the main source of nutrition for joints and their structures. As we all know, people who use public transportation every day and have walking traffic are less likely to develop osteoarthritis.
- Control weight and reduce weight appropriately.The increased mass increases the load on the joints of the lower limbs and spine. Therefore, any osteoarthritis rehabilitation and conservative treatment plan includes an LFT (Physiotherapy Exercises and Gymnastics) course.
- Correction and elimination of congenital deformities.Flat feet play an important role. Over the years, it can cause violations of the axis of the legs, resulting in disproportionate increases in the load on certain parts of the joints and spine, thereby deforming them.
- Good nutrition.It allows you to create conditions to enrich your joints with adequate nutrition. Therefore, a large number of refusal to eat, frequent dieting, irregular low-quality food (fast food, etc. ) nutrition can become the "fuse" of osteoarthritis.
- Eliminate accompanying diseases in time.The now forgotten physical examination makes it possible to detect and eliminate diseases early and in time. Accompanying diseases may be an important reason for the occurrence and development of joint disease (for example, endocrine system disease, gastrointestinal disease, chronic infection focus or inflammation).



















